Dental Insurance
The Dental Plan through Delta Dental provides coverage for preventive, basic and restorative dental services and orthodontia (for children). Three programs are available: PPO, DMO, and Indemnity. The DMO also has coverage for adult orthodontia. Enrollment in dental coverage is voluntary but you may participate starting on your first day of employment if you are a regular employee working at least 20 hours per week.
PPO
Account No. NY04970
The Preferred Provider Organization (PPO) allows you to use a dentist of your choice. If services are received from an in-network provider, your out-of-pocket expenses will be lower than if you use a provider who is not in the network. You may use the Delta Dental Premier or Delta Dental PPO networks. You have an annual deductible and partial reimbursement of expenses. You or your dental provider must submit claims for reimbursement.
Indemnity
Account No. NY04970
In the Indemnity Program, you use dentists of your choice. If services are received from an in-network provider, you will receive a discount on covered services. You may use two networks: Delta Dental Premier and Delta Dental PPO. You have an annual deductible and partial reimbursement of expenses. You or your dental provider must submit claims for reimbursement.
DMO
Account No. NY06503
In the Dental Maintenance Organization (DMO), services are provided through dentists participating in the DeltaCare USA network. There is a schedule of benefits indicating the cost of services. No claim forms are required. You must select a participating dentist for your general dental care, and referrals to specialists are required.
Questions about Delta PPO or Indemnity Program? Call:
(800) 932-0783
Questions about Delta DMO? Call:
(800) 422-4234
Answers to Common Questions
These are answers to the most commonly asked questions about our dental plans. If you need more information, details associated with the dental plans can be found in the Summary Plan Description (PDF).
Signing Up
New employees sign up for coverage by completing an enrollment form within 30 days from your first day of employment. All other eligible employees may sign up for coverage during the Open Enrollment period. You may also be eligible to sign up for coverage if you have a Qualifying Event. See the Qualifying Events section for more information.
Enrolling Your Family
You may enroll your spouse, your unmarried children (through the end of the calendar year in which they attain age 23 including adopted children and stepchildren) who reside with you and are dependent on you for at least half of their support; and your unmarried children age 23 or older who are mentally or physically incapable of self-support (if within 31 days after their 23rd birthday or the date they become incapacitated, whichever occurs first, you submit proof of the incapacity to the Benefits Office and they are approved by the insurance company).
Making a Change to Coverage
If you have a Qualifying Event, you may be eligible to add or drop coverage or dependents at that time. See the Qualifying Events section for more information. You may also change your coverage during the Open Enrollment period, and coverage will be effective January 1 of the following calendar year.
Continuation into Next Year
The elections you have in place for the dental program will roll forward from one year to the next for you and your eligible family members only if all criteria for eligibility are met. For additional information, refer to the Summary Plan Description.
ID Cards
You don't need an ID card to use your dental coverage. Just provide your Name, Life Number, and date of birth to your dentist's office. Here's what to do if you prefer to have a card.
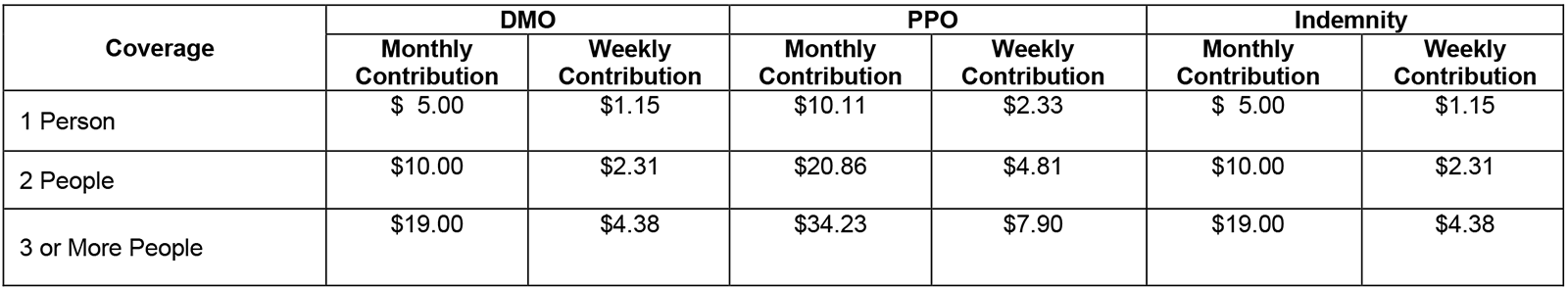
Cost Comparison
2026 Dental Plan Contributions